Radiotherapy for brain tumours in adults
Radiotherapy is a type of treatment that uses radiation to destroy tumour cells. Radiotherapy for a brain tumour can be used on its own, or alongside other treatment options, such as neurosurgery or chemotherapy.
On this page, we’ll discuss:
- What is radiotherapy for brain tumours?
- Before radiotherapy is given
- During radiotherapy
- After radiotherapy
- Radiotherapy FAQs
What is radiotherapy for brain tumours?
Radiotherapy uses controlled doses of invisible, high-energy beams of charged particles (radiation) to destroy tumour cells while causing as little damage as possible to surrounding cells.
It may be used:
- where surgery isn’t possible
- after surgery to kill any remaining tumour cells
- to prevent a tumour from returning
- to slow down the growth of the tumour.
What you might expect from radiotherapy for a brain tumour
Before radiotherapy treatment
Planning your radiotherapy
Your radiotherapy is very carefully planned by a team of medical specialists to make sure it destroys as many tumour cells as possible while damaging the fewest healthy brain cells.
You may have several scans, such as MRI or CT scans. These are to create a 3D image showing the precise location and shape of your tumour to target it more precisely.
The scans also help your healthcare team plan how many sessions of radiotherapy you’ll need and how much radiation to give at each session. This is important as it makes sure that the tumour cells die and that the normal cells have time to recover before the next dose of radiation.
Asking questions
Your healthcare team will also talk through what will happen and discuss any potential side-effects with you before any treatment is given.
This is your chance to ask any questions. Remember, no question is a silly question.
Making your treatment mask
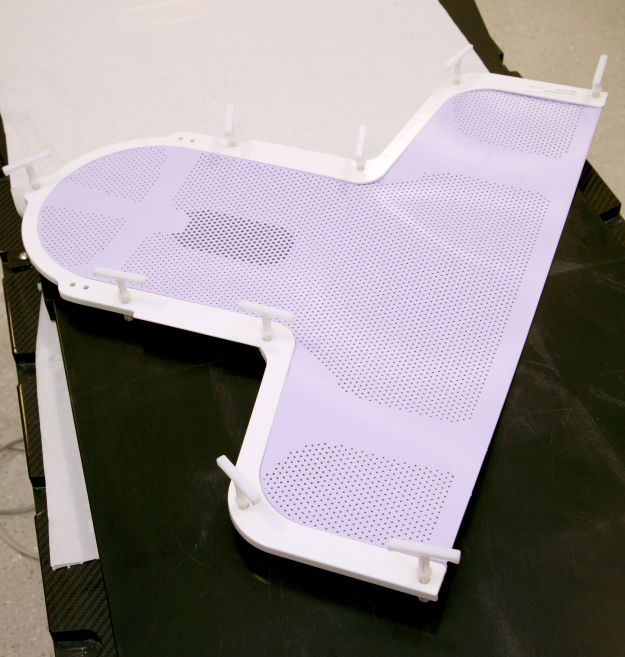
To make sure the radiotherapy is directed to the correct part of your brain, it’s important that you stay very still during the treatment. To help you do this, a tailor-made treatment mask holds your head in position each time you have treatment.
There are different types of mask made from different materials, but you can breathe easily in them and the treatment should be painless. Some people do find wearing a treatment mask claustrophobic. If you feel this way, the therapeutic radiographers who will treat you are skilled at helping with this.
Images reproduced with the kind permission of Cambridge University Hospitals NHS Foundation Trust.




During radiotherapy treatment
Each treatment session is called a ‘fraction’. During each fraction, you’ll lie on a treatment couch wearing your mask, which will be attached to the couch. The radiographers will take a few minutes to make sure you’re positioned correctly, then they’ll leave the room.
They will be able to communicate with you throughout the treatment.
Some radiotherapy machines move around you during treatment while others will look more like a CT scanner.

One of our supporters, Stuart Grant, recorded a time-lapse of a radiotherapy session and has kindly allowed us to share the video to help remove some of the uncertainty people might feel before starting treatment.
Find out more about Stuart’s journey by following @stuartgrantuk on Instagram.
After radiotherapy
Radiotherapy is generally given as an out-patient procedure, so after each session you’ll be able to go home.
It’s likely that you’ll experience some side-effects. Radiotherapy works because it does the greatest damage to rapidly dividing cells. While this includes tumour cells, it also includes rapidly dividing normal cells, such as skin cells, hair cells, cells lining the mouth and the digestive tract, plus blood cells in the bone marrow. These areas, therefore, tend to have the most common side-effects.
You’re also very likely to feel tired both during and after your treatment.
Most side-effects will be temporary and gradually fade, usually within 6-12 weeks after treatment has finished.
Specialist radiographers during the course of your treatment will monitor your side effects and provide help with these.
Following treatment, you’ll have regular check-up appointments, at either your local radiotherapy centre or neurology outpatient service, to monitor the effects of the radiotherapy on your tumour and any side-effects you may get. This is important as long-term side-effects can take months and sometimes years to develop.
Helping you prepare for radiotherapy
Would you like to receive our four-part email guide to your treatment?
If radiotherapy doesn’t work
Although treatment plans are carefully developed by healthcare professionals to be as effective as possible, while having the fewest risks or side-effects, sometimes radiotherapy may not work.
This can be worrying, but just because one treatment hasn’t worked, it doesn’t mean others won’t.
Frequently asked questions
-
Each treatment is called a ‘fraction’. Each fraction can be between a few seconds to a few minutes. Your appointment, however, will be considerably longer, as medical staff will take time making sure you’re in the right place.
The period of time over which your radiotherapy is spread varies from person to person, but it’s common for it to last for around 4-6 weeks.
An example of a typical radiotherapy plan is treatment once a day, Monday to Friday, with a break at the weekends.
Before the treatment begins, your medical team will be able to tell you how many sessions you’ll need, how often and over what period. They’ll also be able to give you a guideline for how long each visit to the hospital should take.
-
No, you can’t feel radiotherapy nor is there any heat from it. The machine can be quite noisy though.
-
Generally, you’ll be given radiotherapy as an outpatient, which means going into the hospital for each fraction, after which you can go home.
A stay might be needed if you are also receiving chemotherapy, or if you are unwell.
-
It is likely that you will have to take some time off work during treatment and for a short time afterwards. Side-effects, such as tiredness and nausea, may mean you need a longer period of time off work.
Our employment resources provide help and information on how to approach your employer about your diagnosis and how they can support you through this time.
-
No. The radiation comes from the machine and does not stay inside your body. You don’t need to take special precautions when you leave the hospital. It’s safe to be around others, including children.
-
Radiotherapy is given in a way to minimise the chance of permanent side-effects. However, some effects, such as hair loss, may last.
Occasionally some side-effects of radiotherapy may be longer-term or develop later in life, depending on how much and which areas of your brain have been treated.
-
Your full dosage of radiation is carefully calculated, depending partly on the size, type and location of the tumour. It is then divided into fractions for two reasons.
Firstly, depending on where a cell is in its growth cycle, it can be more or less sensitive to radiation. By giving radiotherapy in several doses, it makes sure the tumour cells receive radiation when they’re most sensitive.
Having a gap between doses also gives healthy cells time to recover between treatments, while still causing damage to the tumour cells, which are more sensitive to radiation.
By joining one of our Online Support Groups, you can get more tips about living with or beyond a brain tumour diagnosis from people who truly understand what you’re going through.
Support and Information Services
Research & Clinical Trials Information
You can also join our active online community.
In this section

Get support
If you need someone to talk to or advice on where to get help, our Support and Information team is available by phone, email or live-chat.
Recommended reading
Share your experiences and help create change
By taking part in our Improving Brain Tumour Care surveys and sharing your experiences, you can help us improve treatment and care for everyone affected by a brain tumour.